Advertisement for health workers only
Chronicle: Stig Slordahlmanaging director Helse Midt-Norge RHF
HE it’s hard to disagree with Norwegian Medical Association president Marit Hermansen, who recently wrote that we have one of the best health services in the world. He admitted he was concerned about “imminent dark clouds” with increasing social inequalities in health and emerging divisions in health services.
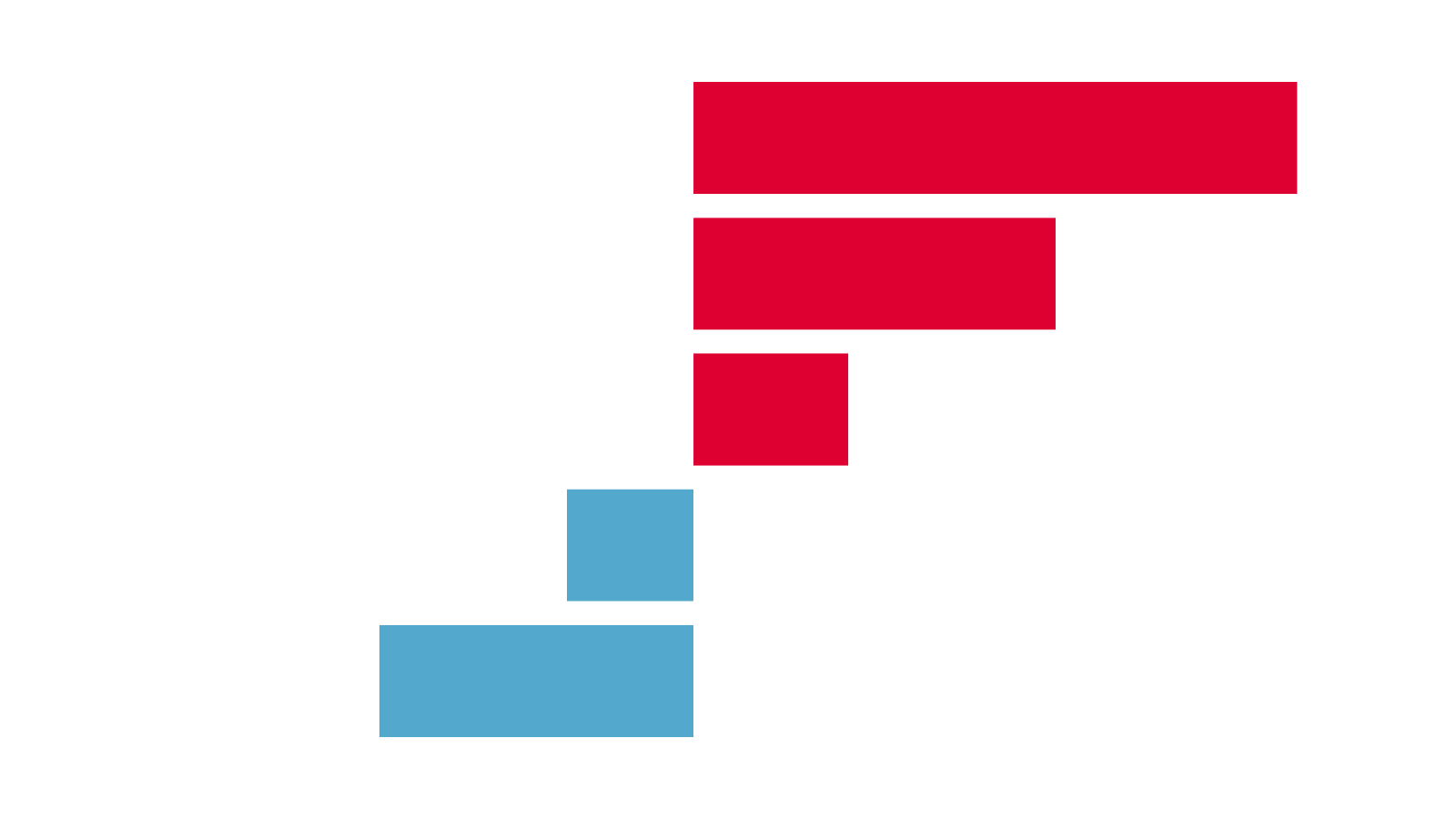
In July, a report came from the American foundation The Commonwealth Fund, which compared health services in 11 rich countries – Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom and the United Kingdom. United States of America. Unsurprisingly, the United States scored worst despite the fact that no other country spends as much on health. Norway shares fourth place with New Zealand, beaten by Great Britain, Australia and the Netherlands.
DIFFERENT SYSTEMS. For many people, it may come as a surprise that the UK with its National Health Service (NHS) comes out on top in such a comparison. They achieved the highest marks in all areas apart from the outcomes achieved by health services. Here, Norway is in third place. There are nine areas that are assessed in order to be able to convey the quality of health services in the areas of outcomes such as infant mortality rate, life expectancy for those who reach the age of 60 years, 30-day mortality rate for those who have reached the age of 60 years. hospitalization for heart attack and stroke, and five-year relative survival for breast cancer and colon cancer.
Interestingly, the three countries at the top of the ranking have very different health systems. It is true that these countries have universal health coverage, which means the entire population has access to health services. In the UK, health services are paid for through tax revenues and central government has an important role in organizing and running health services. Most hospitals are government hospitals with civil servants, while primary care practices are mostly privately owned.
COVERAGE. In Australia, everyone is covered by an insurance scheme and funded like the NHS through tax revenues, but the public sector has a smaller role in running health services. Most hospitals are private, and about half the population has private insurance to access health services outside the government system.
In the Netherlands, citizens are required to purchase private health insurance. Insurance companies are required to provide health insurance to everyone who applies and must contain mandatory sections similar to the services we offer in our system. Financing consists of two parts, an income-dependent part paid into a mutual fund and a part paid directly to the insurance company. Transfers then occur between the pooled funds and individual insurance companies based on the risk profile of those applying for insurance.
Advertisement for health workers only
ORGANIZATION. Norway ranked second to last in the area of “process of care”, which should be relevant to healthcare as a whole – prevention, patient safety, coordination, patient engagement and patient preferences. Perhaps these results reflect some of the challenges we face in dividing health services into specialist health services, municipal health services and general practitioners.
I have written in previous columns that Norway would never have the health service we have if we started today. Then we will start from what is appropriate for the patient and society as a whole.
Patients think they are dealing with one health service – and we must organize ourselves so that they experience it as one health service. A good start would be to compensate for such fragmentation through new funding arrangements and common record-keeping solutions such as the Health Platform Plan in Central Norway. In a health service, we must properly maintain the competence, perspective and authority of primary health services – including general practitioners.
LIFT IT TO THE ENTIRETY. We feel very fortunate in Norway to have such skilled and professionally committed doctors. In this regard, the emerging signals about poor recruitment for general practitioner jobs are now worrying. There may be several different reasons for this. In Denmark, it is also difficult to get young doctors to invest and establish themselves in municipal governments, while various private companies open medical practices after taking part in municipal tenders, and reportedly have fewer problems employing young doctors on a fixed salary. Perhaps the time has come to consider more public service and a fixed wage.
Going forward, it will be important to prioritize the parts of health services that need improvement to ensure the whole. Over the past few years, we have experienced a large and necessary growth in specialist health services without, for example, strengthening the tenure of doctors in municipalities. Additionally, specialist health services may need to better support what happens in primary health care.
TAKE A LESSON! We agree that we have – and will continue to have – a strong, high-quality public health service in Norway. However, we must be able to learn from what is happening in other countries so that we can continue to develop. Of course, we must work to combat social inequalities and divisions in health care, but we must also put health into a broader perspective.
We will not succeed if social inequality increases generally and politics does not support improving public health. Good public health is more than just good health services.
Chronicles and debates, Dagens Medisin 14/2017

“Social media guru. Total beer fanatic. Tv ninja. Typical coffee fan. Amateur entrepreneur. Unapologetic food scholar.”